Vaginal Surgery Kansas City
 A prolapse occurs when surrounding organs or structures push into your vaginal canal, often causing urinary problems, bowel symptoms, and sexual dysfunction, among other issues. If you’re struggling with a prolapse, Patrick Nosti, MD, FACOG, at Urogynecology of Kansas City, offers innovative treatment solutions. Find out more by booking a prolapse evaluation today.
A prolapse occurs when surrounding organs or structures push into your vaginal canal, often causing urinary problems, bowel symptoms, and sexual dysfunction, among other issues. If you’re struggling with a prolapse, Patrick Nosti, MD, FACOG, at Urogynecology of Kansas City, offers innovative treatment solutions. Find out more by booking a prolapse evaluation today.
UROGYNECOLOGY OF KANSAS CITY | 913.262.3000
Apical Suspensions
Apical suspension surgery restores the support of the top of the vagina, which is also called the vaginal apex or vault, and helps to maintain sexual function. There are several procedures that address the apex.
Sacral Colpopexy
The sacral colpopexy can be performed through an abdominal incision (about 3 to 4 inches long), laparoscopically (through 4 half-inch incisions), or robotically. For more details regarding this procedure, please click “robotic surgery”.
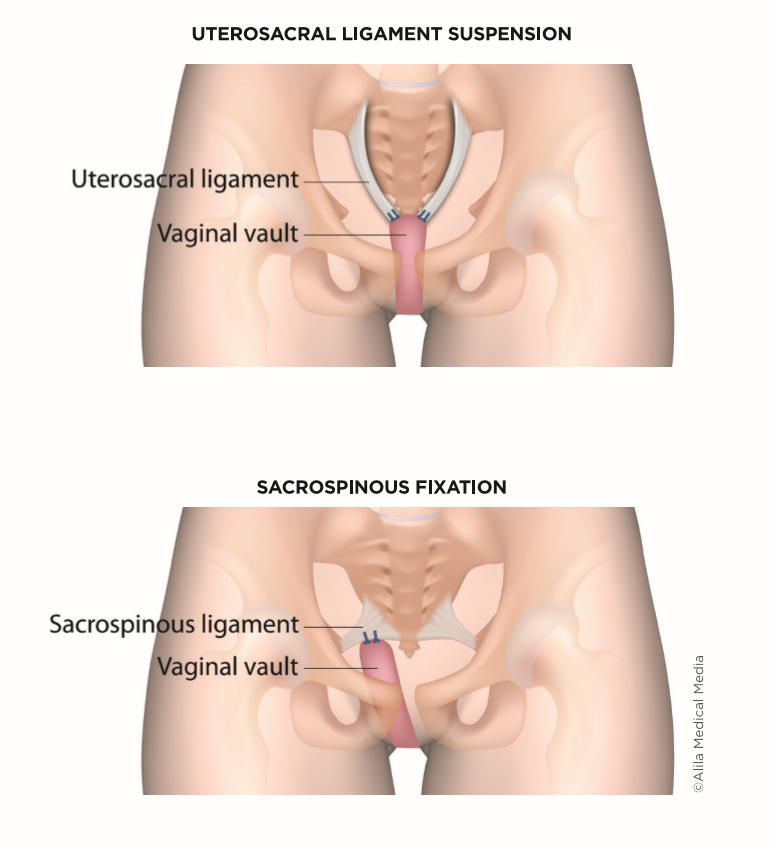
Uterosacral or Sacrospinous Ligament Fixation
When a vaginal incision is preferred, the top of the vagina is most often suspended to a woman’s own uterosacral ligament or the sacrospinous ligaments. Traditionally, these procedures do not use graft material.
Anterior Vaginal Prolapse Repair
A cystocele or bulge of the front wall of the vagina usually results in a loss of support for the bladder that rests upon this part of the vagina. The goal of a cystocele repair is to elevate the anterior vaginal wall back into the body and support the bladder. This can be done either vaginally, called anterior colporrhaphy, or through an abdominal approach at the time of a sacral colpopexy.
Anterior colporrhaphy is a commonly performed repair of a cystocele. In anterior colporrhaphy, an incision is made in the front wall of the vagina. The vaginal skin is separated from the bladder wall behind it. The weak or frayed edges of the deep vaginal wall are found, and the strong tissue next to the edges is sutured to each other, lifting the bladder and recreating the strong ”wall” underneath it. The vaginal incision is then closed with dissolving stitches.
Posterior Vaginal Prolapse Repair
A rectocele or bulge of the back wall of the vagina is most often repaired by a vaginal procedure called posterior colporrhaphy. If the muscles at the opening of the vagina have been stretched or separated during childbirth, the repair may include a perineorrhaphy. A rectocele may also be fixed abdominally at the time of a sacral colpopexy.
Posterior Colporrhaphy
Posterior colporrhaphy is a procedure that repairs the rectal bulge protruding through the back wall of the vagina.
During the colporrhaphy procedure, an incision is made in the back wall of the vagina. The vaginal skin is separated from the rectal wall underneath. The weak or frayed edges of the deep vaginal wall tissue are identified. The strong tissue next to the edges is sutured to each other, creating the strong ”wall” between the rectum and the vagina. The vaginal incision is then closed.
Perineorrhaphy
Surgical reconstruction of the muscles of the perineum, the area between the vagina and the rectum. This procedure involves reattaching a number of small muscles that normally connect in this area.
Obliterative Procedures
For those women who do not desire to maintain sexual function, an obliterative procedure may be the quickest and least risky method to correct prolapse. Obliterative operations correct prolapse by narrowing and shortening the vagina. These procedures support the pelvic organs with the patient’s own pelvic muscles in such a way as to make the vagina too small to accommodate a penis for sexual intercourse.
The skin overlying the vaginal bulge is removed, and the front and back walls of the vagina are sewn to each other. A woman who has undergone this surgery will look the same on the outside of her genital area, and she will be able to have bowel movements and urinate normally. Her ability to have an orgasm with clitoral stimulation is similar to before her surgery.
There are two main types of obliterative surgery:
- Partial (colpocleisis).
- Complete (colpectomy).
Both are very effective and durable in correcting prolapse. Prior surgeries often influence which procedure is offered to women. The benefit of obliterative surgery is that it is very durable, does not involve the risks of graft materials, tends to be less invasive, and therefore is associated with a quicker recovery.
Related Reviews
Very Professional | 5.0 
“I appreciate Dr. Nosti and his staff for helping me. They were all very professional and kind during appointments and answering my questions. I was confident in Dr. Nosti’s ability to perform my surgery.“
Review from Angela S. | Source: Google | April 25th, 2022
Total vaginal hysterectomy
During a total vaginal hysterectomy, the uterus is surgically removed through the vagina. The operation is frequently combined with prolapse repair of the bladder and/or bowel. There are no abdominal or laparoscopic incisions. A vaginal hysterectomy offers many benefits over abdominal or laparoscopic procedures. It offers overall fewer complications, a shorter healing time, less pain, less scarring, a lower chance of infection, a lower risk of hernias, and a faster return to activities. Also, a prolapsed uterus is easier to access via the vagina. The operation is performed in a hospital setting and can be performed under general or spinal anesthesia (with or without sedation). A cut is made around the cervix. The surgeon then carefully pushes the bowel and bladder away from the uterus. The blood vessels supplying the uterus and surrounding tissue are then clamped and secured. After confirming that there is no bleeding, the surgeon removes the uterus and closes the top of the vagina, now known as the vaginal vault.
In the context of prolapse, the surgeon will add additional support stitches to the vaginal vault at the time of surgery, either to the uterosacral ligaments that support the uterus (this is called a uterosacral ligament suspension) or to support structures on the side of the uterus (this is called a sacrospinous ligament suspension or ileococcygeus suspension).
Oophorectomy
Before surgery, the woman and her surgeon decide whether the ovaries and/or the fallopian tubes should be removed and whether estrogen replacement therapy is needed.
Removal of ovaries: A hysterectomy does not involve removing the ovaries, but they may be removed at the same time as a hysterectomy; this procedure is known as an oophorectomy. The decision to remove the ovaries depends on several considerations. Occasionally, it may not be possible to remove the ovaries due to scar tissue or other factors that increase the risk of removal. If the ovaries are removed at the time of the hysterectomy, the fallopian tubes will be removed as well.
Premenopausal women may decide to keep the ovaries to provide a continued, natural source of hormones, including estrogen, progesterone, and testosterone. These hormones are important in maintaining sexual interest and preventing hot flashes and bone density loss. On the other hand, some women who have menstrual cycle-related migraines, epilepsy, or severe premenstrual syndrome may have an improvement in symptoms when hormone levels are reduced by the removal of the ovaries. Individuals should discuss the risks and preferences with a doctor before surgery.
Older postmenopausal women are usually advised to have their ovaries removed because of a small risk of developing ovarian cancer at some point during their lifetime. This benefit of removing the ovaries appears to outweigh the benefit of continued hormone production, as described above.
Women in the menopausal transition (called “perimenopause”) and in earlier menopause, typically between 45 and 65 years of age, should discuss with their clinicians their individual risks for keeping their ovaries versus having them removed. Increasing evidence suggests that the small number of hormones produced by the ovaries during this perimenopausal period may improve heart and bone health.
Removal of fallopian tubes: It is possible to remove the fallopian tubes with a hysterectomy but leave behind the ovaries. Removing the fallopian tubes may decrease the small risk of later developing one type of ovarian cancer while preserving the hormone production of the ovaries. Occasionally, it may not be possible to remove the fallopian tubes due to scar tissue or other factors that increase the risk of removal.
How Much Does Treatment for Vaginal Prolapse Cost?
As symptoms and triggers vary greatly from one patient to another, Vaginal Prolapse treatments are also varied. Once we have formulated a treatment approach for you, we will review your treatment plan and price details with you.
Schedule a Consultation
Schedule your consultation for treatment of Vaginal Prolapse in Kansas. Contact Dr. Nosti and set up your appointment. During your appointment, you will be able to ask questions and bring up any concerns you may have about the procedure. Contact us today to get the look you’ve always wanted!